
At least 40 million Americans each year suffer from chronic, long-term sleep disorders, and an additional 20 million experience occasional sleep problems. Of the 70 known sleep disorders, the most common are:
Insomnia, the most prevalent of the sleep disorders, is characterized by an inability to fall asleep and/or by waking up during the night and having difficulty going back to sleep.
Obstructive sleep apnea (OSA) is a potentially life-threatening disorder in which breathing is interrupted during sleep. An estimated 12 million Americans have OSA.
Restless leg syndrome (RLS) is a neurological movement disorder that often is associated with unpleasant leg sensations and an almost irresistible urge to move the legs,
Narcolepsy is a chronic disorder characterized by excessive and overwhelming daytime sleepiness, even after adequate nighttime sleep. Daytime sleep attacks may occur with it or without warning and may be uncontrollable.
Many Americans struggle through episodes of sleep disorders on their own, while others may use over-the-counter drugs, prescription drugs, or sleeping devices to combat them. A growing number of people are seeking Upper Cervical Care with great success while avoiding the potential side effects or dependence on outside means.
Sleep & Overall Health
People spend about one-third of their lives asleep. Nonetheless, people generally know little about the importance of sleep. They do agree, however, it is absolutely essential for good physical and mental health and for survival.
Loss of sleep creates an overwhelming, and sometimes uncontrollable, need to sleep and affects virtually all physiological functions. Problem sleepiness is associated with difficulty concentrating, memory lapses, complex thought, loss of energy, fatigue, lethargy, impaired motor response and emotional instability. Problem sleepiness can even be deadly. Approximately 100,000 automobile accidents each year result from drivers who were “asleep at the wheel.”
The functions of many organ systems are linked to sleep cycles, like the endocrine system (hormone secretion), the renal system (blood filtering), and alimentary activity (digestion). Studies also show that sleep deprivation affects the immune system in detrimental ways. In addition, sleep loss can alter temperature regulation and increase the risk for various physical and mental disorders.
Sleep & The Brain Stem
Sleep is a highly organized sequence of events that follows a regular, cyclic program each night. It is controlled and coordinated in the brain stem and brain. The brain stem region, known as the pons, is critical for initiating REM sleep (the dream cycle).
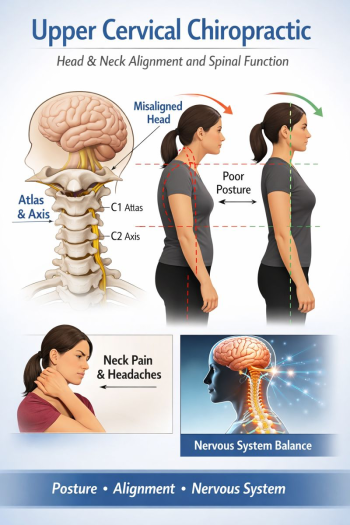
The brain stem, which can be compared to a telephone cable with thousands of individual wires or nerve fibers sending signals between the brain and the body, controls nearly all vital, bodily functions. Misalignments in the upper cervical spine (neck) can affect the function of the brain stem, which can be a critical factor in many health problems including sleep disorders.
Misalignments may be caused by a number if things, including bumps, falls, car accidents, and emotional stress, just to name a few. Health problems may appear immediately after the injury or several years later.
Upper Cervical Chiropractic Care & Sleep Disorders
Upper Cervical doctors are getting exceptional results with patients suffering from sleep disturbances. Clinical trials and case studies document the improvement in patients with sleep disorders while receiving Upper Cervical Chiropractic Care.
Dr. Jerome Ri, DC is an Upper Cervical Doctor of Chiropractic, located in Huntington Beach, who has extensive training and education in the brain stem and upper cervical spine. He has dedicated his professional life to helping patients with pain, sickness, and disease.
If you suffer from a sleep disorder and would like to seek the help of Dr. Ri, call (714) 848-8122 to schedule a no-cost consultation. Or you can use the Contact Page to request a consultation online.
Upper Cervical Care has “given life back” to countless sleep disorder sufferers. Dr Ri knows how to develop a program specific to your needs. Most health insurance companies recognize the benefits of upper cervical care and include it among the services they cover.
Get Your Life Back!
At least 40 million Americans each year suffer from chronic, long-term sleep disorders, and an additional 20 million experience occasional sleep problems.
References & Case Studies
Amalu, W., et al. Applied Upper Cervical Biomechanics Course. International Upper Cervical Chiropractic Association, Redwood City, CA 1993.
Amico G, Pasquali F, Pittaluga E. Pickwickian-narcoleptic disorders after brain concussion. Riv Sper Freniatr Med Leg Alien Ment 1972 Feb 29; 96(1): 74-85.
Arky, R., et al., Physicians’ Desk Reference(PDR). Montvale, NJ. Medical Economics Data Production Co., 2003.
Barrette K, Buxton N, Redmond AD. Comparison symptoms experienced following minor head injury and acute neck strain (whiplash injury). J Accid Emerg Med 1995 Sep;12(3):173-6.
Beetar JT, Guilmette TJ, Sparadeo FR. Sleep and pain complaints in symptomatic traumatic brain injury and neurologic populations, Arch Phys Med Rehabil 1996 Dec; 77(12) 1298-302.
Blair Upper Cervical Chiropractic Certification. Palmer College Of Chiropractic, Davenport, IA 2005.
Di Stefano G, Radanov BP. Neuropsychological and psychosocial findings in follow-up of cervical vertebrae dislocations: a prospective clinical study. Z Unfallchir Versicherungsmed 1993; 86(2): 97-108.
Eriksen, K: Upper Cervical Subluxation Complex – A Review of the Chiropractic and Medical Literature. Baltimore, MD, Lippincott, Williams & Wilkins, 2004.
Ettlin TM, Kischka U, Reichmann S. Cerebral symptoms after whiplash injury of the neck: a prospective clinical and neuropsychological study of whiplash injury. J Neurol Neurosurg Psychiatry 1992 Oct; 55(10):943-8.
Fichtenburg NL, Millis SR, Mann NR Factors associated with insomnia among post-acute traumatic brain injury survivors. Brain Inj 2000 Jul;14(7):659-67.
Fichtenburg NL, Putnam SH, Mann NR. Insomnia screening in post acute traumatic brain injury: utility and validity of the Pittsburgh Sleep Quality Index. AM J Phys Med Rehabil 2001 May; 80(5): 339-45.
George B, Landau-Ferey J, Benoit O. Night sleep disorders during recovery of severe head injuries, Neurochirurgie 1981; 27(1):35-8.
Grostic, JD. Dentate Ligament-Cord Distortion Hypothesis. Chiro Research J, 1988; 1(1):47-55.
Guilleminault C, Yuen KM, Gulevich MG. Hypersomnia after head-neck trauma: a medicolegal dilemma. Neurology 2000 Feb 8; 54(3): 653-9.
Guyton, A., Hall, J.: Textbook of Medical Physiology. Philadephia, W.B. Saunders Co., 2000.
Henry GK, Groos HS, Herndon CA. Nonimpact brain injury: Neuropsychological and behavioral correlates with consideration of physiological findings. Appl Neuropsychol 2000; 7(2): 65-75.
Kale, MU. Kale Certification Residency Program. Spartanburg, SC, 2004.
Landau-Ferey J, George B. Benoit O. Polygraphic study of nocturnal waking in patients with traumatic brain stem injuries. Rev Electroencephalogr Neurophysiol Clin 1981 Sep; 11(1): 116-22.
Lishman WA. The psychiatric sequelae of head injury: a review. Psychol Med 1973 Aug; 3(3): 304-18
Mayou R, Bryant B, Duthie R. Psychiatric consequences of road traffic accidents. BMJ 1993 Sep 11; 307(6905): 647-51.
Miller LS, Garde IB, Moses JA. Head injury and mood disturbance. J Clin Psychiatry 1992 May; 53(5): 171-2.
National Upper Cervical Chiropractic Association and Guidelines and Standards of Care. NUCCA. Monroe:1997.
Nemoto M, Akino M, Abe H. Atlantoaxial dislocation with ventilatory insufficiency-report of two cases. No To Shinkei 1996 Feb; 48(2): 155-60.
Nizamie SH, Nizamie A, Borde M. Mania following head injury: case reports and neuropsychological findings. Acta Psychiatr Scand 1988 Jun; 77(6): 637-9.
Palmer, B.J.: Chiropractic Clinical Controlled Research, Vol.XXV. W.B.Cronkey Company, Hammond, IN, 1996 (reprint)
Palmer, B.J. Subluxation Specific, Adjustment Specific, VOL. XVIII. 1991 (reprint)
Patten SB, Lauderdale WM. Delayed sleep phase disorder after traumatic brain injury. J AM Acad Child Adolesc Psychiatry 1992 Jan; 31(1):100-2.
Quinto C, Gellido C, Chokreverty S. Post traumatic delayed sleep phase syndrome. Neurology 2000 Jan 11; 54(1): 250-2.
Schreiber S, Klag E. Gross Y. Beneficial effect of risperidone on sleep disturbance and psychosis following traumatic brain injury. Int Clin Psychopharmacol 1998 Nov; 13(6): 273-5.
Smed A. Cognitive function and distress after common whiplash injury. Acta Neurol Scand 1997 Feb; 95(2): 73-80.
Sweat, RW. Atlas Orthogonal Board Certification, Life University, Atlanta, GA, 2005.
Taylor AE, Cox CA, Mailis A. Persistent neuropsychological deficits following whiplash: evidence for chronic mild traumatic brain injury: Arch Phys Med Rehabil 1996 Jun; 77(6): 529-35.
Tierney, L.M., et al.: Current Medical Diagnosis and Treatment 2005, 44th Edition. New York, NY, Lange Medical Books/McGraw-Hill, 2005.
Tobe EH, Schneider JS, Mrozik T. Persisting insomnia following traumatic brain injury. J Neuropsychiatry Clin Neurosci 1999 Fall; 11(4): 504-6.
Upper Cervical Diplomate Program, Sherman College of Straight Chiropractic. Spartanburg, SC, 2005.
Webb M, Kirker JG. Severe post-traumatic insomnia treated with L-5-hydroxytrytophan. Lancet 1981 Jun 20; 1(8234): 1365-6.
Webster JB, Bell KR, Hussey JD. Sleep apnea in adults with traumatic brain injury: a preliminary investigation. Arch Phys Med Rehabil 2001 Mar;82(3):316-21.
Wilcox JA, Nasrallah HA. Childhood head trauma and psychosis. Psychiatry Res 1987 Aug; 21(4): 303-6.
Zwil AS, McAllister TW, Cohen I, Halpern LR. Ultra-rapid cycling bipolar affective disorder following a closed-head injury. Brain Inj 1993 Mar-Apr; 7(2): 147-52.



Leave a comment